At-home Detection of Heart Failure
Heart failure is a leading cause of death worldwide and now researchers hope to combat it in a whole way. They have developed a point-of-care electrochemical biosensor that can measure levels of two biomarkers for heart failure in as little as 15 minutes from just a drop of saliva.
“Our device would be ideal for people, who are at high risk for heart failure but have limited access to a hospital or a centralized lab,” said developer Trey Pittman, who is with Colorado State University, Fort Collins, Colorado. “Working on this project to address health disparities in rural and low-resource areas really hits home for me because I’m from Mississippi, which has one of the highest mortality rates from heart failure in the United States.”
Heart failure refers to weakened heart muscle that cannot pump enough oxygenated blood through the body. The current gold standard for heart failure screening is a blood test administered twice per year by a healthcare professional. It measures levels of B-type natriuretic peptide (BNP), a protein that indicates the heart is working too hard.
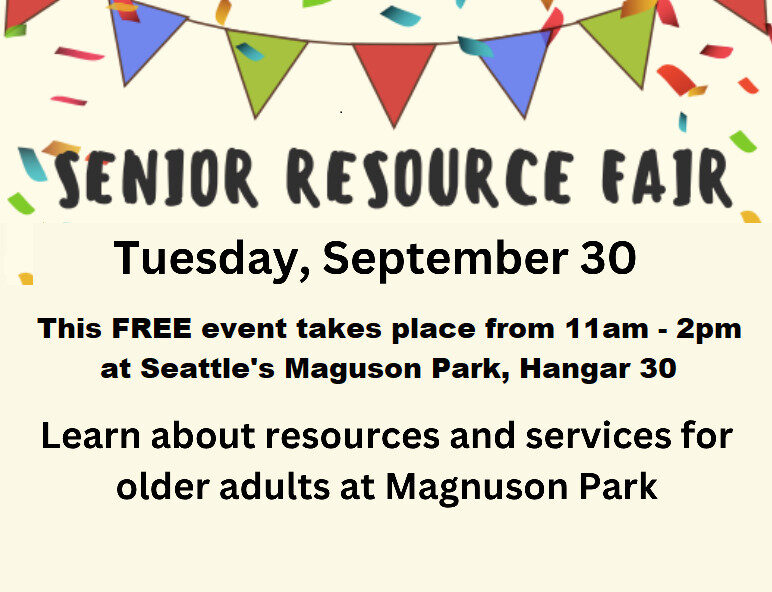
Now, a simple, at-home saliva test may soon change things. It could be used to check an older adult every few weeks instead of every six months, suggests Pittman. So far, widespread use of portable saliva tests for heart health has been limited by complicated manufacturing techniques and lack of relevant data beyond the presence or absence of a single biomarker. No word yet on when this saliva test will be commercially available.
Bombastic Bandages Battling Infections
New research on wound care at Binghamton University in New York is combining a biodegradable paper dressing that uses bacteria-fueled biobatteries. This technique begins with therapeutic dressings that inhibit dangerous biofilms. These dressings are applied with paper and contain spore-forming bacteria that produce antibacterial agents along with electrical stimulation powered by biobatteries.
The team has successfully added copper oxide and tin oxide nanoparticles to the spore-carrying bacteria to generate a tiny amount of power. When channeled into the wound area, the electric current seems to break down the cell integrity of the infecting microbes and stimulate healing. The researchers tested their paper-based dressing on simulated human skin and pig skin with promising results, but more investigation is required before the process is ready for human use.
Principal investigator Sean Choe with Binghamton University said biodegradable papertonics and bacteria-fuel biobatteries may usher in a new way to treat a host of diseases. “The beauty of using paper is that it is disposable, so you don’t need to worry about a second infection after you use it, but the future work is necessary,” said Choi.
While this research is very promising, it is still in early development stages. Choe said there are still many unanswered questions. “We don’t clearly understand how this electrical stimulation heals the wound infections. One guess is that the membranes of bacterial cells were damaged, but the type of electrical stimulation or how long in duration or how frequently to make it effective is something we need to study further.”
Wirelessly Monitoring in the ER
Physicians in the emergency department (ED) at Vanderbilt University Hospital (VUH) are now using wireless physiologic monitoring. The new rechargeable device is from a company called Masimo. The device’s central unit, the size of a bath-sized bar of soap, attaches to the person’s lower arm. Sensors run to the hand, upper arm, chest and neck.
Besides displaying vital signs on a small screen on the device’s central unit, it also connects to the hospital network using the local wireless Wi-Fi network protocol. Data flows to the patient record and is displayed on centrally located electronic boards where doctors can keep an eye on the patient’s status. When vital signs change, automatic alarms are triggered. Patients can get up to use the bathroom without having to unhook from a monitor.
“Wireless monitoring promises both to enhance support for our care teams and to elevate care for patients placed in our nontraditional spaces and in our waiting room,” said Dr. Ian Jones an associate professor of Emergency Medicine and a clinical director with HealthIT at Vanderbilt University Medical Center, Nashville, Tennessee. “This is an innovative measure aimed at improving vigilance, efficiency and satisfaction for patients and staff.”
The pilot extends to continuous wireless monitoring of blood pressure, blood oxygen level (pulse oximetry), heart rate, and, in selected patients, continuous cardiac rhythm. Patients in standard ED beds at VUH are tethered to plug-in monitors that are wired to the VUMC network, allowing continuous central monitoring and automatic alarms when vital signs change. Those beds and their patients are outside the scope of the ED’s wireless initiative.
Hallway beds are used for arriving patients who may be less in need of a standard ED bed. While these patients may generally be more stable than those in standard beds, care standards still call for periodic checking of their vital signs. “In bringing wireless physiologic monitoring to the ED, we’re providing more surveillance, more vigilance to each patient’s physiologic status. Technology such as this forms part of the solution as health care systems such as ours seek to make care better and more efficient.,” said Dr Neal Patel, a professor of Clinical Informatics and chief informatics officer for HealthIT at Vanderbilt University.
John Schieszer is an award-winning national journalist and radio and podcast broadcaster of The Medical Minute. He can be reached at medicalminutes@gmail.com.