Marci’s Medicare Answers - February 2014
January 31, 2014 at 12:00 a.m.
Dear Marci,
I switched to a different Medicare prescription drug plan during the Fall Open Enrollment Period in 2013. Unfortunately, a drug that I had been taking regularly since 2010 will not be covered by my current drug plan. Is there any way I can get my drug covered by my current plan?
—Roscoe
Dear Roscoe,
Yes. If your new Medicare prescription drug plan, also known as a Part D plan, does not cover a drug that you had already been taking, your plan should provide you with a 30-day transition fill at some time during the first 90 days of the year. A transition fill is a one-time, 30-day supply of a Medicare-covered drug that Medicare prescription drug plans must cover when you’re in a new plan or when your existing plan changes its coverage. Note that transition fills are not for new prescriptions. In order to get a transition fill, you must have been taking the drug before switching your Part D coverage or before your existing plan changed its drug coverage.
In addition to providing you with the transition fill, Part D plans must also give you a transition notice explaining that you are currently using your transition fill and informing you of your appeal rights. If your drug is covered on your new Part D plan’s list of covered drugs (i.e. formulary), but the plan has imposed coverage restrictions on the drug (e.g. step therapy or prior authorization), your plan must give you a 30-day transition fill without restrictions during the first 90 days you are enrolled in the plan.
Note that getting a transition fill is a temporary solution. In order to ensure that you are able to get your drugs throughout the year, you should contact your doctor right away. Ask your doctor if he/she can make an exception request to your plan and formally ask your new plan to cover your drug so that your drug can be covered throughout the year. Also, consider talking to your doctor about switching you to a drug that your plan does cover.
—Marci
Dear Marci,
Friends have told me that Medicare now covers mental health care in the same way that it covers other types of health care. Is this true?
—Suzanne
Dear Suzanne,
Yes. In 2013, Original Medicare, the traditional Medicare program administered by the federal government, covered 65 percent of the cost of the Medicare-approved amount for outpatient mental health visits. In 2013, people with Original Medicare insurance were responsible for the cost of the remaining 35 percent coinsurance if they did not have any sort of Medigap supplemental insurance to pay for that coinsurance.
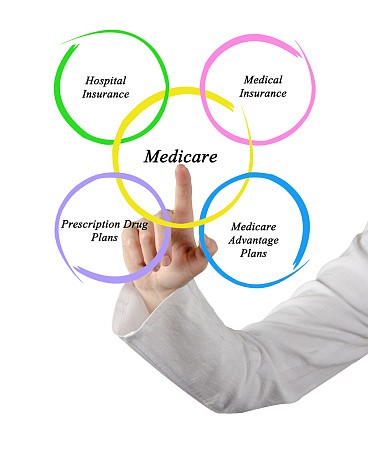
In 2014, Original Medicare began covering 80 percent of the cost of the Medicare-approved amount for outpatient mental health visits in the same way that it covers 80 percent of the Medicare-approved amount for most outpatient services. Keep in mind, however, that Original Medicare has not changed how it covers inpatient mental health services. If you receive care in a psychiatric hospital, Medicare covers up to 190 days of inpatient care in one lifetime. After you have reached that 190-day limit, Medicare may pay for mental health care at a general hospital. Your inpatient psychiatric hospital costs will be the same as the inpatient hospital costs you pay under Original Medicare Part A, the hospital insurance part of Medicare.
If you have a Medicare Advantage plan, also known as a Medicare private health plan, know that different costs and rules may apply. Contact your plan directly to learn more about your plan’s coverage of outpatient mental health benefits.
—Marci
Dear Marci,
I received a notice in the mail from the Centers for Medicare & Medicaid Services. This notice is telling me that the Medicare Advantage plan I’ve enrolled in is a consistently low-performing plan. What does this mean?
—Marcia
Dear Marcia,
In early February, the Centers for Medicare & Medicaid Services (CMS) sends notices to people who have recently enrolled in a consistently low-performing Medicare Advantage or Part D plan. CMS will send this notice to you if your plan has received an overall Medicare star rating of less than three stars for three consecutive years.
Medicare star ratings are quality ratings for Medicare Advantage and Part D plans. Each year, Medicare scores how well plans perform in several categories, including quality of care and customer service. Star ratings range from one to five stars, with five being the highest score and one being the lowest score. Medicare also assigns plans one overall star rating to summarize the plan’s performance as a whole.
If you have received this notice, you are entitled to a Special Enrollment Period (SEP) to disenroll from the low-performing plan and enroll into a Medicare Advantage or Part D plan with an overall star rating of three stars or more. You will be able to make this switch once at anytime during the rest of the year. To use this SEP, you will need to call 800-MEDICARE directly.
If you do not want to make any changes and you want to stay in your current plan, you will be allowed to do so; however, you should make sure that the plan’s costs, coverage benefits and rules will best meet your individual needs for the remainder of the year.
Lastly, keep in mind that people with Medicare are also allowed an SEP to enroll into a five-star Medicare Advantage plan or Part D plan once each calendar year. In order to use this SEP, the plan must have an overall five-star rating and must be offered in your service area. Note that this five-star SEP is separate from the SEP you are entitled to if you are in a consistently low-performing plan.
To learn more about a particular plan’s star rating or to locate higher quality plans in your area, you can call 800-MEDICARE or go online and visit www.medicare.gov/find-a-plan.
—Marci
Marci’s Medicare Answers is a service of the Medicare Rights Center (www.medicarerights.org), the nation’s largest independent source of information and assistance for people with Medicare. To subscribe to “Dear Marci,” MRC’s free educational e-newsletter, click here.